InsideOut eLearning
Learn more about eating disorders with our suite of online courses for health professionals.
eLearning
Initial Medical Assessment
Concerns should always be taken seriously
An initial assessment requires a combination of medical and psychological assessment.
At the initial appointment it is important to:
- Assess risk - eating disorders are associated with serious physical and psychiatric complications
- Book in follow-up appointment - to monitor ongoing risk and conduct further medical investigations (see Medical monitoring)
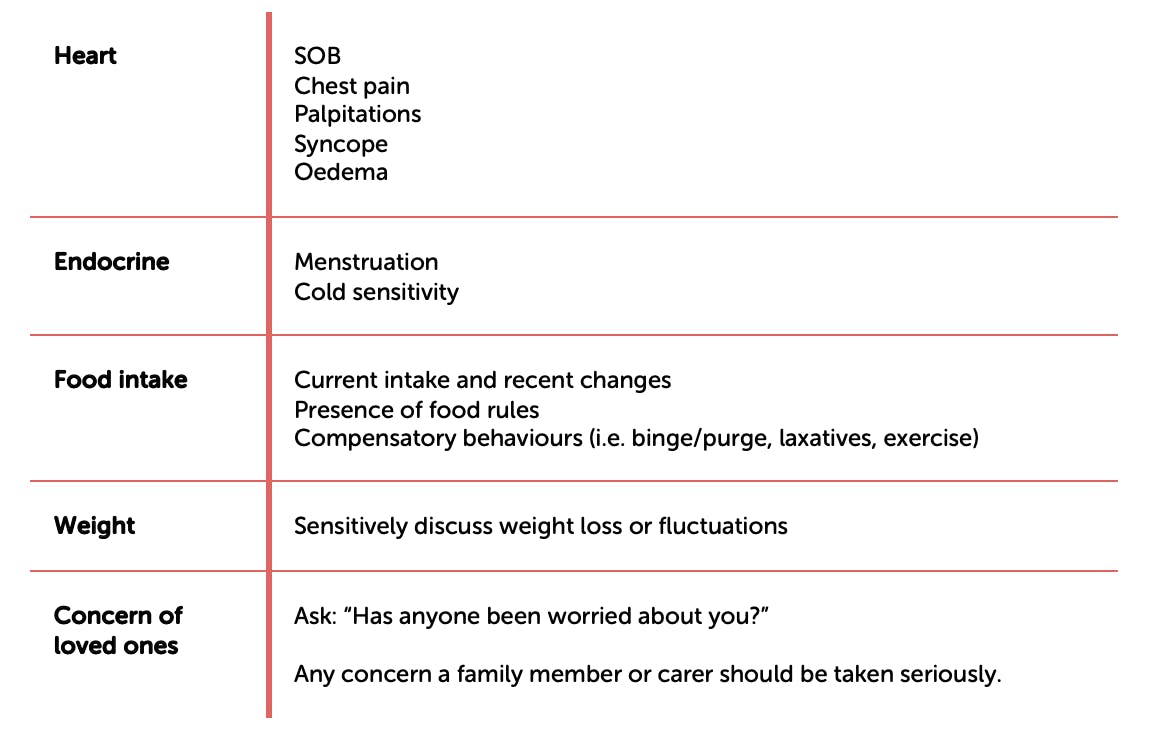
History / Assess Risk:
Physical Exam:
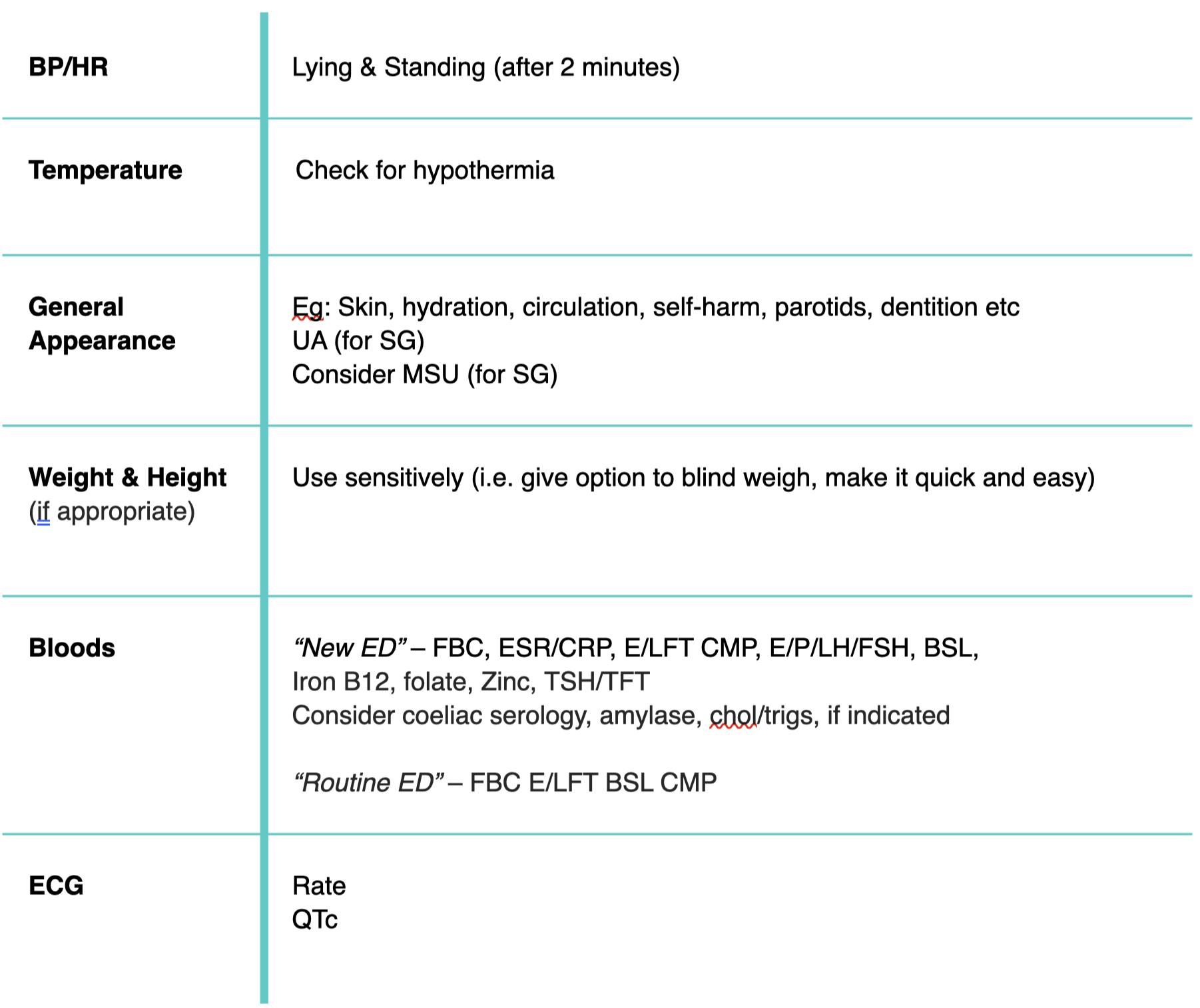
Ensure that any physical exam is carried out sensitively. It can be highly distressing for a person with severe body image disturbance to expose their body to an unfamiliar person.
GP Practice Management Toolkit
Customise your software with autofill templates and patient info
Other signs to look out for:
- Skin Examination
Look for acrocyanosis (blue discolouration), jaundice, carotenaemia (orange skin), dry skin, hair loss/thinning, lanugo hair (soft downy hair on back, arms), callused knuckles (repeated induced vomiting), skin infections and lesions from self-harm
- Assessment for dehydration
Look for sunken eyes, dry lips and tongue, poor skin turgor and slow capillary return
- Oral Examination
Look for signs that may occur with recurrent vomiting. These include dental erosions, pharyngeal redness and parotid enlargement
- Assessment for signs of vomiting
Look out for swollen parotid glands, recurrent sore throat, bouts of tonsillitis, halitosis, callused knuckles (repeated induced vomiting), bloodshot eyes and broken capillaries in the cheeks and eyelids
- Assessment of cardiovascular / respiratory systems
It is important to assess blood pressure (seated and standing). A fall or rise of 10-20 beats per minute on standing indicates cardiac compromise. Heart rate (seated and standing), bradycardia/tachycardia on minimal exertion indicates deconditioning. Core temperature, shortness of breath (orthopnoea, paroxysmal nocturnal dyspnoea, exercise tolerance), palpitations (sudden onset, frequency, duration), chest pain (onset, frequency, duration, associated symptoms, precipitating factors), examination of peripheries (circulation, coldness in hands and feet, oedema) and fainting, collapse, light-headedness, dizziness
- Assessment of gastrointestinal and renal systems
Assess for delayed gastric emptying (causes prolonged fullness), post prandial symptoms (distension, abdominal pain, bloating and early satiety), reflux, diarrhoea, constipation and urinalysis
- Assessment of musculoskeletal system
Assess for stress fractures, overuse injuries and bone mineral density if indicated.
- Assessment of menstrual disturbances
Although primarily considered a manifestation of low weight or malnutrition, amenorrhea can be associated with many factors including prolonged weight loss, erratic eating behaviours, poor nutrition, excessive exercise and stress, and can occur irrespective of the individuals weight.