InsideOut eLearning
Learn more about eating disorders with our suite of online courses for health professionals.
eLearning
Rejected from Emergency
Patient was rejected from the emergency department: What now?
People with eating disorders are not always admitted to hospital, despite the urgent need for inpatient care.
Psychiatrist Prof. Janice Russell discusses what to do when a patient is knocked back from the emergency department.
For indicators that require urgent hospital admission see: Is This An Emergency?
What to do when you think that someone should be in hospital, but is not or cannot be admitted:
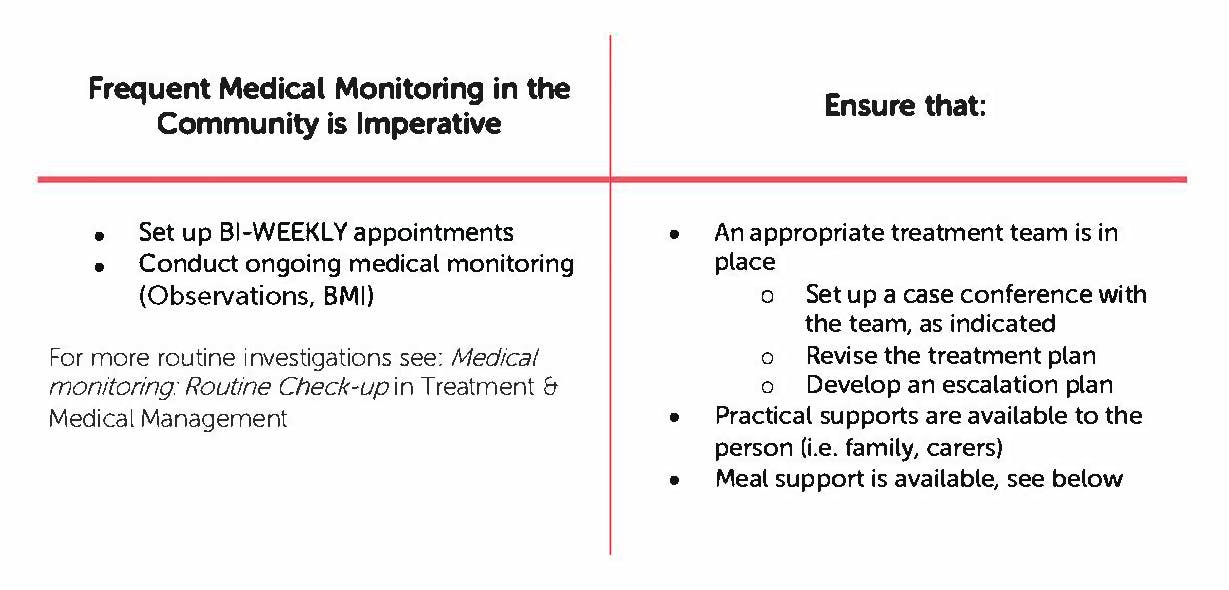
Important things to consider:
- Multi-vitamin and thiamine
- Risk of refeeding (low but can be mitigated), see below
- Work through further investigations, as indicated, at own pace. See: Medical Monitoring: Routine Check-up and Medical Monitoring: Body Systems.
- Medications
- SSRIs may be beneficial in the treatment of co-occurring depression and obsessive-compulsive disorder. Low dose of olanzepine may be helpful in anorexia nervosa, when patients are severely anxious and demonstrate obsessive eating-related ruminations. See also: Treatment Evidence Planning Tool
- Liaise with local specialist services - let them know what you can and cannot manage
Psychiatrist Prof. Janice Russell discusses steps to safely refeed a patient in need of urgent care.
Eating Disorder Coordinator
New South Wales, and several other jurisdictions, have an organised system for helping people with eating disorders access treatment and stepped care treatment options, including hospital.
In NSW, there is an Eating Disorder Coordinator in every health district. The Eating Disorder Coordinator can assist you in establishing treatment pathways, escalate care if needed, provide support and find specialist eating disorder professionals. Please see our website for contact details for your local Eating Disorder Coordinator
Remember: GPs have the skills and knowledge to care for people with EDs. Many routine practices are applicable and just need to be modified.